Explore This Guide
- Why Week 5 Earns the "Most Critical" Title
- The Developmental Milestones: A Week-by-Week Snapshot of the First Trimester
- What's Happening in Your Body During This Critical Time?
- Common Concerns and What They Really Mean
- Your Action Plan: What To Do (and Not Do) During This Pivotal Week
- Answering Your Burning Questions (The FAQ Section)
- Beyond Week 5: The Rest of the First Trimester Journey
- Final Thoughts: Navigating the Critical Early Weeks with Confidence
So you just found out you're pregnant. Congratulations! The whirlwind of emotions is probably hitting you – excitement, nervousness, a bit of disbelief. And then come the questions. So many questions. One of the biggest ones that pops up for a lot of women, once the initial shock wears off, is this: what is the most critical week of the first trimester? It's a search I see all the time in forums and groups. Everyone wants to know when they need to be extra, extra careful.
Here's the thing. The entire first trimester is a period of rapid, miraculous, and incredibly delicate development. Calling one week "the" most critical feels a bit like picking the most important piece of a watch – they all need to work together. But if we're talking about a pivotal moment, a point where the foundation is laid and the trajectory is set, then hands down, the consensus points to Week 5.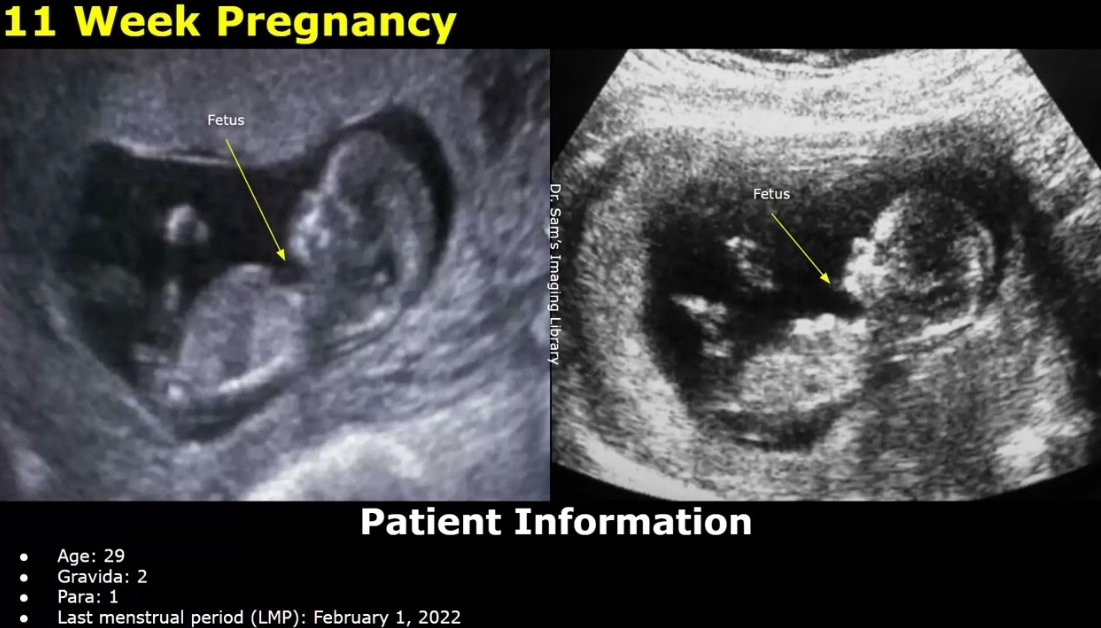
Why Week 5? Because this is when the embryo transitions from a tiny cluster of cells to something that starts resembling a tiny human. It's the week of the "primitive streak" and the beginning of gastrulation – big words for the process where the basic layers of your baby's future body are formed. Mess this up, and the whole developmental plan can go awry. So, when asking what is the most critical week of the first trimester, Week 5 is the heavyweight contender.
I remember with my first, I was blissfully unaware. I was just tired and my breasts were sore. It wasn't until my first ultrasound and the doctor pointed to the little flicker of a heartbeat and said, "Look at that! All the major organ systems are starting to form now," that the gravity of it hit me. That was Week 7, but the real magic, the silent, invisible heavy lifting, had happened two weeks prior.
Why Week 5 Earns the "Most Critical" Title
Let's break it down without the medical textbook jargon. Think of the first four weeks as the planning and zoning phase. The sperm met the egg, they formed a blastocyst, and it implanted in your uterine wall. Important, sure, but it's mostly about getting settled.
Then Week 5 arrives. The embryo, now about the size of an apple seed, isn't just sitting there. It's a construction site working three shifts. This is when the neural tube begins to form. This tube will eventually become your baby's brain, spinal cord, and backbone. If this tube doesn't close properly by the end of Week 6, it can lead to neural tube defects like spina bifida.
But it's not just the nervous system. The cardiovascular system is also kicking off. The very first version of the heart starts to develop and will soon begin to beat (usually visible around Week 6). The foundations for the digestive tract, the early kidneys, and the limb buds (those will be arms and legs!) are all being sketched out.
So, the reason the most critical week of the first trimester is often cited as Week 5 is because it's a period of high susceptibility. The cells are rapidly dividing and differentiating, and they are incredibly sensitive to disruptions. Teratogens (things that can cause birth defects) like certain medications, high levels of radiation, or severe nutritional deficiencies can have their most profound impact during this window.
It's a sobering thought, but it's also empowering. Knowing this gives you a clear focus for your care.
The Developmental Milestones: A Week-by-Week Snapshot of the First Trimester
To really understand why Week 5 stands out, it helps to see it in context. Here's a quick look at what's happening before and after. You'll see how Week 5 acts as the crucial launchpad.
| Week | What's Happening with Baby | Key Vulnerability / Note |
|---|---|---|
| Week 4 | Implantation completes. The blastocyst splits into embryo and placenta cells. | Chemical pregnancy risk is highest. Many women don't yet know they're pregnant. |
| Week 5 | Neural tube formation begins. Primitive heart and circulatory system start. Gastrulation (layer formation) occurs. | PEAK susceptibility to major structural birth defects. Neural tube must close in the coming week. |
| Week 6 | Heart begins to beat (visible on ultrasound). Limb buds appear. Neural tube should close. | Critical period for heart and limb development continues. |
| Week 7-8 | Major organs (brain, lungs, liver, kidneys) continue rapid development. Facial features form. | Organogenesis in full swing. Still a highly sensitive period. |
| Week 9-12 | Organs mature and begin to function. Fingers and toes separate. Bones harden. | Sensitivity to teratogens decreases, but brain development remains vulnerable. |
See the pattern? Week 5 is the ignition switch. It's the week that sets in motion the processes that define the next seven months. That's a pretty solid argument for it being the most critical week of the first trimester.
What's Happening in Your Body During This Critical Time?
While the embryo is busy with its mega-construction project, your body is going through its own dramatic changes to support it. And honestly, some of these changes are what make you realize something's up, even before a missed period for some.
Progesterone and hCG (human chorionic gonadotropin) levels are skyrocketing. This hormonal surge is responsible for many of the classic early pregnancy symptoms. You might be experiencing:
- Fatigue that hits like a truck. This isn't normal tiredness. It's a deep, bone-weary exhaustion because your body is using massive amounts of energy to build a placenta and support that embryonic growth spurt.
- Breast tenderness and swelling. They might feel heavy, sore, or tingly.
- The dawn of morning sickness. Nausea can start as early as Week 5 for many women. It's misnamed, of course – it can strike any time of day or night. The cause isn't entirely clear, but those high hCG levels are a prime suspect.
- Frequent urination. Your kidneys are working more efficiently, and your growing uterus is starting to press on your bladder, even at this tiny size.
- Food aversions or cravings. Suddenly, the smell of coffee you used to love makes you gag. Or you have an intense desire for pickles at 2 AM.
The weird thing is, some women feel absolutely nothing. And that's normal too. The absence of symptoms doesn't mean something is wrong. Every body handles the hormonal shift differently. But if you are feeling rotten, try to take it as a sign that those hormones are doing their job, supporting that critical development in Week 5.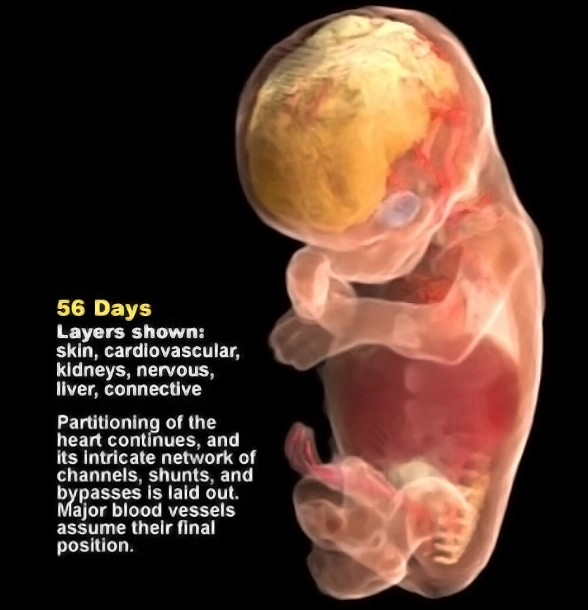
Common Concerns and What They Really Mean
This period is also fraught with anxiety. Every twinge, every cramp, every time you run to the bathroom to check for spotting, your mind races. Let's address some of the big fears head-on.
Cramping: Mild, period-like cramping is very common as your uterus begins to stretch and expand. It's usually nothing to worry about. Severe, sharp, one-sided pain is a different story and warrants a call to your doctor.
Spotting: A few drops of pink or brown blood can be normal implantation bleeding (if it's very early) or just cervical irritation. Heavy bleeding, like a period, with cramping is more concerning and should be evaluated.
Lack of symptoms: As mentioned, it's not a bad sign. Consider yourself lucky for now!
The mental load is real. You're trying to process this huge life change while worrying about every little physical sensation. It's exhausting on another level. Knowing that you're in the most critical week of the first trimester can amplify that anxiety. The key is to focus on what you can control.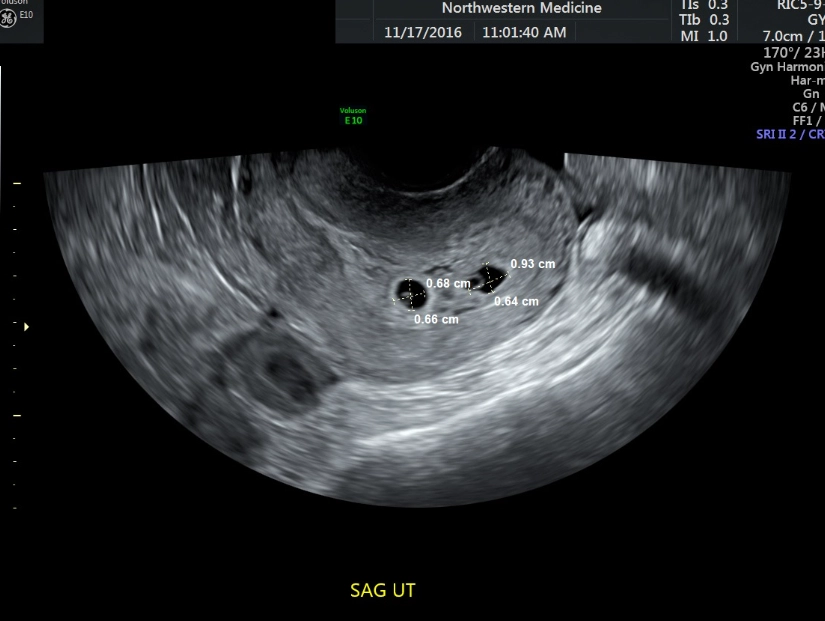
Your Action Plan: What To Do (and Not Do) During This Pivotal Week
Knowledge is power, but action is comfort. Now that you know what is the most critical week of the first trimester, here's your practical guide for navigating it. This isn't about living in fear; it's about making informed choices to give your little one the best possible start.
The Must-Do List for Weeks 5-6
- Start or Continue Prenatal Vitamins: This is non-negotiable. The folic acid in prenatal vitamins is crucial for preventing neural tube defects. The CDC recommends all women of childbearing age take 400 mcg of folic acid daily, and this becomes even more critical once you're pregnant. If you haven't started, start today. The CDC has clear guidelines on this.
- Schedule Your First Prenatal Appointment: Call your OB-GYN or midwife. Many won't see you until 8-10 weeks, but getting on the calendar is important. They'll give you specific instructions and answer your initial questions.
- Evaluate Your Diet: You're not "eating for two" in terms of calories yet, but you are eating for the quality of two. Focus on whole foods: fruits, vegetables, lean proteins, whole grains, and healthy fats. Hydrate, hydrate, hydrate.
- Listen to Your Body: If you're exhausted, rest. Seriously. Your body is doing immense work. A 20-minute nap can be a game-changer.
The "Be Very Careful" List
- Avoid Alcohol, Smoking, and Recreational Drugs: There is no known safe amount of alcohol during pregnancy, and this is the most vulnerable time for its effects. Smoking restricts oxygen and nutrients. Just don't.
- Review Your Medications: Talk to your doctor about any prescription or over-the-counter meds you take. This includes supplements and herbal remedies. Some common drugs (like certain acne medications or some pain relievers) are not safe during early pregnancy.
- Food Safety: Skip the sushi, unpasteurized cheeses (like brie, feta, queso fresco), deli meats unless heated steaming hot, and raw cookie dough. These can harbor bacteria like listeria, which, while rare, can have severe consequences during pregnancy.
- Limit Caffeine: Most experts agree that under 200 mg of caffeine per day (about one 12-oz coffee) is likely safe, but more than that may be linked to increased miscarriage risk, especially in the first trimester. I switched to half-caff and then mostly to herbal tea during my first tri, just to be safe.
One thing I wish someone had told me: the housework can wait. The social obligations you don't feel up for can be canceled. Your primary job right now is to grow a human and survive the first trimester. Everything else is secondary. Giving yourself that permission is a form of self-care.
Answering Your Burning Questions (The FAQ Section)
You'll have a million questions. Write them down. Bring the list to your first appointment. A good healthcare provider won't mind.
Beyond Week 5: The Rest of the First Trimester Journey
While we've crowned Week 5 as the most critical week of the first trimester, the weeks that follow are no less important. They're just different. From Week 6 to Week 12, it's all about refinement and growth.
The heart is now beating and pumping blood. Tiny fingers and toes are forming and separating. The brain is developing at an astonishing rate. By the end of the first trimester, your baby has all its major organs, muscles, and nerves, and is starting to practice moving (though you won't feel it for weeks).
The risk of major structural defects decreases significantly after Week 10, as the organs are mostly formed. However, the brain and nervous system continue to be vulnerable to certain insults (like alcohol) throughout the entire pregnancy.
So, while the intense, foundational construction phase of the most critical week of the first trimester is over, you're moving into the phase of intricate interior design and system testing. It's all vital.
Final Thoughts: Navigating the Critical Early Weeks with Confidence
So, what is the most critical week of the first trimester? We've landed on Week 5. It's the week where the master plan is executed, where the neural tube forms, and the heart begins its lifelong work.
Knowing this isn't meant to scare you.
It's meant to empower you. It gives context to the fatigue and nausea. It underscores the importance of that prenatal vitamin. It explains why your doctor asks about your last menstrual period with such precision.
The first trimester is a season of secrecy and survival for many. You might not be telling the world yet, you might feel awful, and you're likely worried. That's normal. Be gentle with yourself. Make the best choices you can with the information you have. Take your vitamin, eat as well as you can stomach, rest when you need to, and communicate with your healthcare provider.
You've got this. You're already doing an incredible job by seeking out information and wanting to understand this miraculous, critical process. One week, one day, one nap at a time.