Let's cut through the noise. You've probably heard the statistic: fertility declines after 35. Maybe you've seen the scary headlines about "geriatric pregnancy." It creates this looming, often silent anxiety. Is there a concrete age limit for having a baby? The short, honest answer is no, there's no law or single age that slams a door shut. But medicine paints a picture of shifting probabilities, not absolutes. This guide isn't about fear; it's about power through information. We're going past the clichés to look at what really changes with age, the specific tests you need to know about, and how to navigate your options with clear eyes.
What's Inside This Guide
How Does Age Actually Affect Pregnancy? It’s More Than Just a Number
Think of it like this: your eggs are with you from birth. They age as you age. This isn't about your overall health or fitness—you can run marathons at 40—but about cellular changes in the eggs themselves. The most significant impact is on chromosomal normality.
As eggs age, the chance of errors during division increases. This leads to a higher probability of chromosomal conditions, the most common being Down syndrome (Trisomy 21). The numbers tell a clear story. Look at this risk progression, which is often cited in genetic counseling and by sources like the American College of Obstetricians and Gynecologists (ACOG):
| Maternal Age at Delivery | Approximate Risk of Down Syndrome | Key Medical Designation |
|---|---|---|
| 25 | 1 in 1,250 | Standard Risk |
| 30 | 1 in 952 | Standard Risk |
| 35 | 1 in 385 | Advanced Maternal Age (AMA) |
| 40 | 1 in 106 | AMA |
| 45 | 1 in 30 | AMA |
That "Advanced Maternal Age" label kicks in at 35. It sounds awful, I know. In my practice, I've seen women get the paperwork and flinch. But medically, it's just a trigger for a different standard of care. It means your doctor's protocol changes.
Beyond chromosomes, other risks see a gradual increase:
- Miscarriage: The rate climbs, largely linked to those chromosomal issues. By age 40, the risk is about 35%; by 45, it can be over 50%.
- Gestational Diabetes & High Blood Pressure: Your body's metabolic and vascular systems may not handle the stress of pregnancy as easily. Screening happens earlier and more often.
- Cesarean Delivery: Rates are higher, often due to a combination of factors like increased monitoring and a higher incidence of conditions that make vaginal delivery riskier.
- Multiple Pregnancy: This one's ironic. The rate of fraternal twins actually peaks in the late 30s due to hormonal shifts, before declining again.
What Are the Essential Medical Tests for a Pregnancy Over 35?
If you're pregnant at an advanced maternal age, your prenatal care isn't just about checkups. It's a diagnostic journey. You'll hear about a menu of tests. Here’s what they really mean, stripped of jargon.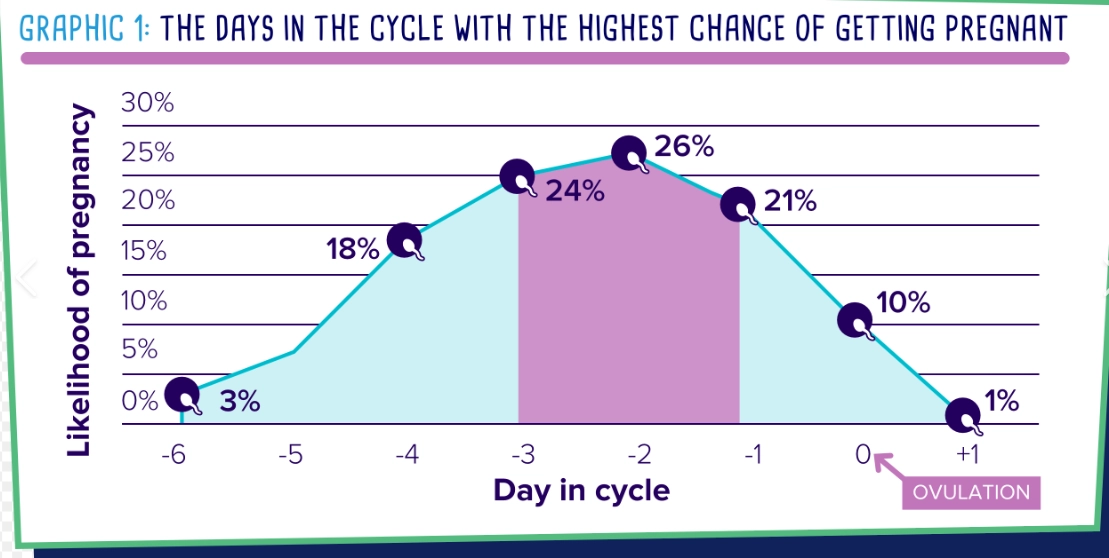
The Screening Powerhouse: NIPT (Non-Invasive Prenatal Testing)
This is a blood test you can get after 10 weeks. It analyzes fetal DNA floating in your bloodstream to screen for major chromosomal issues. Its accuracy for conditions like Down syndrome is very high, often over 99%. For women over 35, this is often the first major test. The crucial thing to understand? It's a screen, not a diagnosis. A "high risk" result means you need the next step.
The Diagnostic Gold Standards: CVS and Amniocentesis
This is where I see the biggest knowledge gap. Many hope NIPT is enough. It's not, if you need certainty.
- Chorionic Villus Sampling (CVS): Done between 10-13 weeks. A thin tube takes a tiny sample of placental tissue. It gives a definitive chromosomal answer early, which is a huge pro for decision-making.
- Amniocentesis: Done after 15 weeks. A thin needle withdraws a small amount of amniotic fluid. Also definitive. It has a slightly lower miscarriage risk than CVS (about 1 in 500 to 1 in 1000 when done by an expert), but you wait longer for results.
The miscarriage risk of these procedures is the elephant in the room. The often-cited 1 in 300-500 figure is outdated for experienced practitioners at major centers. The real risk is closer to 1 in 800-1000. You must weigh this tiny risk against the risk of the condition you're testing for (see the table above). At 45, the risk of a chromosomal issue (1 in 30) is magnitudes higher than the procedure risk.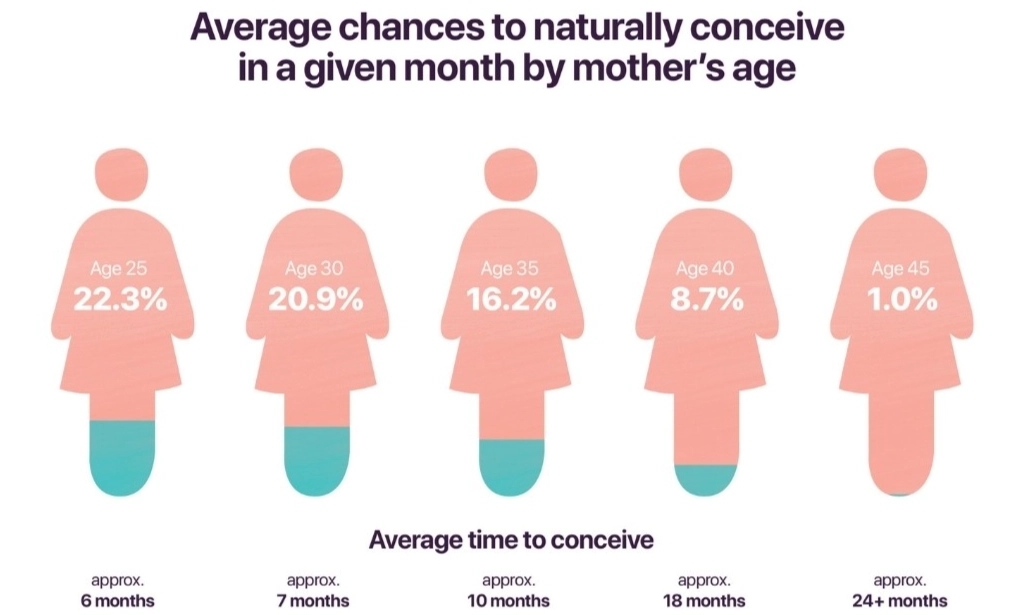
Other tests become non-negotiable:
- Early and Frequent Glucose Testing: For gestational diabetes, often done at the end of the first trimester, not the standard 24-28 weeks.
- Detailed Anatomy Ultrasound (Level 2): Around 20 weeks, performed by a maternal-fetal medicine specialist to check for physical development markers.
- Growth Ultrasounds in the Third Trimester: To ensure the baby is growing properly, as growth restriction risks are higher.
Navigating Your Path and Options
So you're thinking about pregnancy at 38, or 42. What's the actual game plan? It breaks down into phases.
The Pre-Conception Phase (The Most Important Step Most Skip)
Don't just start trying. Get intelligence first. A pre-conception visit with an OB-GYN or reproductive endocrinologist is critical. They'll likely recommend:
- Ovarian Reserve Testing: Blood tests for AMH (Anti-Müllerian Hormone) and a Day 3 FSH/Estradiol, plus an Antral Follicle Count via ultrasound. This gives a snapshot of your egg supply.
- A Full Health Workup: Thyroid, blood pressure, weight management. Getting these optimized is like tuning an engine before a long trip.
This phase tells you if you have a year to try naturally or if you should consider assisted reproduction sooner. It removes the guesswork.
When to Consider Fertility Treatment
The general rule of thumb shifts with age. Under 35, try for a year. At 35-40, try for 6 months. Over 40, many experts recommend an evaluation after 3 months of unsuccessful trying. Time is the one resource you can't get back.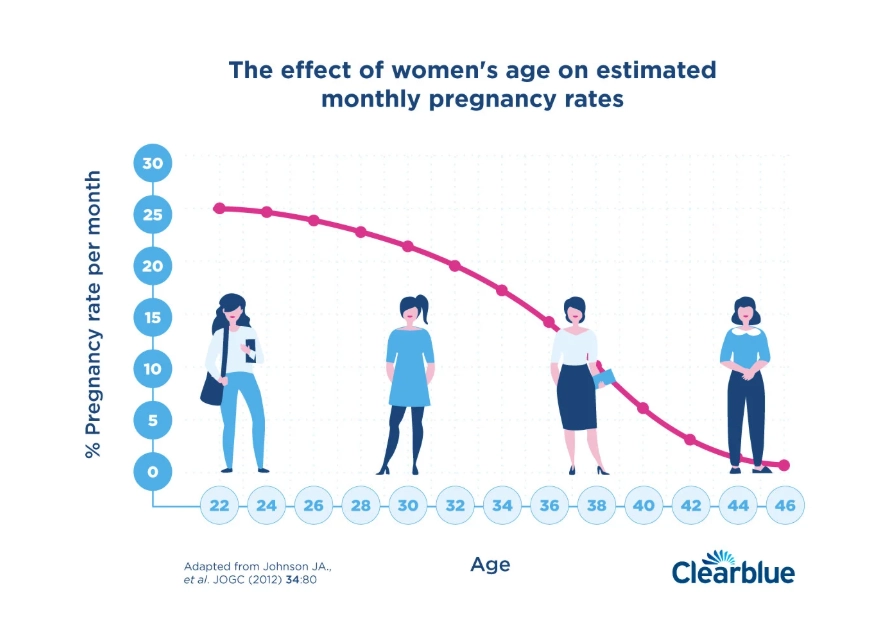
Treatments escalate:
- IUI (Intrauterine Insemination): Can help if timing is the only issue.
- IVF (In Vitro Fertilization): The big tool. It allows for embryo creation and, critically, PGT-A (Preimplantation Genetic Testing for Aneuploidy). This tests embryos for chromosomal normality before transfer, dramatically increasing the chance of a successful pregnancy and reducing miscarriage risk. For women over 38, PGT-A is often a game-changer.
- Donor Eggs: This is a profound decision. When a woman's own eggs have a very high rate of abnormality (common after 42-43), using eggs from a younger, screened donor offers a high chance of a healthy pregnancy. The baby will be genetically related to the father and carried by the mother. It's not a first step, but for many, it's the step that leads to a family.
The Emotional and Practical Guide They Don't Give You
The medical stuff is one thing. The rest is what you live with. Let's talk about it.
You'll feel isolated sometimes. Your friends who had kids at 30 might not get the extra anxiety of every test. You might feel judged for "waiting too long." Find your community—online forums for "AMA moms" or local groups. They get it.
Prepare for the physical reality. Pregnancy at 40 is often more exhausting than at 30. Your back might ache more. Give yourself permission to rest without guilt. Hire help if you can—a cleaner, a meal service. This isn't indulgence; it's strategic energy management.
Have the hard conversations early. With your partner: What will we do if the CVS shows a serious condition? What is our limit for fertility treatments? With your employer: What are my leave options? Getting aligned reduces crisis-mode decision-making.
I remember a patient, Sarah, who conceived naturally at 43 after two rounds of failed IVF. Her pregnancy was medically textbook but emotionally taxing. Her support system of other "later-in-life" moms was her lifeline. They celebrated the small wins differently.
Your Questions, Answered by Reality
 There's no magic age that ends the possibility of pregnancy. There's only a landscape of changing odds, medical protocols, and personal choices. The goal isn't to scare you away but to equip you. Knowledge turns anxiety into agency. Whether you're 35 and just starting to think about it, or 42 and deep in the process, understanding the real limits—and the real options—is how you write your own story.
There's no magic age that ends the possibility of pregnancy. There's only a landscape of changing odds, medical protocols, and personal choices. The goal isn't to scare you away but to equip you. Knowledge turns anxiety into agency. Whether you're 35 and just starting to think about it, or 42 and deep in the process, understanding the real limits—and the real options—is how you write your own story.