In This Guide
- Why Bother Learning to Read the Report Yourself?
- The Anatomy of Your Ultrasound Report: A Section-by-Section Breakdown
- Decoding Common (and Confusing) Medical Terminology
- What's Normal? Understanding Ranges and Variations
- Questions to Ask Your Doctor After Your Ultrasound
- When to Seek Clarification (and When to Relax)
So you just had your ultrasound. The technician was nice, you saw some blurry black-and-white shapes moving on the screen (was that a foot? A nose?), and you got a few cute pictures to take home. Then, they hand you a printout or you see the report later in your patient portal. It’s full of abbreviations, numbers, and medical jargon that might as well be in another language. Sound familiar?
I remember staring at my first report, feeling a mix of awe and total confusion. I could see my baby, but what did all those numbers mean? Was the “EFW” good? Why did it say “anterior placenta”? I spent hours googling terms, which was a mistake—it just led me down rabbit holes of worry. That’s why I wanted to put this together. This isn’t a medical textbook. It’s a plain-English, step-by-step walkthrough to help you decode that document yourself, so you can have a more informed chat with your doctor and feel a lot less in the dark.
Let’s be clear from the start: your doctor or midwife is your ultimate resource for interpreting your specific results. This guide is to empower you, not replace them. Think of it as your translator.
Why Bother Learning to Read the Report Yourself?
You might wonder, "If my doctor will explain it, why should I learn?" Fair question. In an ideal world, your provider would have all the time in the world to sit with you and explain every single line. The reality is often different. Appointments can be rushed. You might forget to ask a crucial question in the moment, or the answers might not sink in until you're home, staring at the paper again.
When you understand the basics of how to read your pregnancy ultrasound report, you shift from being a passive recipient of information to an active participant in your care. You can ask better questions. You won't panic over a normal variant. You'll know what's truly important to focus on. It gives you a sense of control during a time when so much feels out of your hands.
The Anatomy of Your Ultrasound Report: A Section-by-Section Breakdown
Most reports follow a similar structure, though the exact headings can vary by clinic or hospital. Let's break down the typical sections you'll encounter.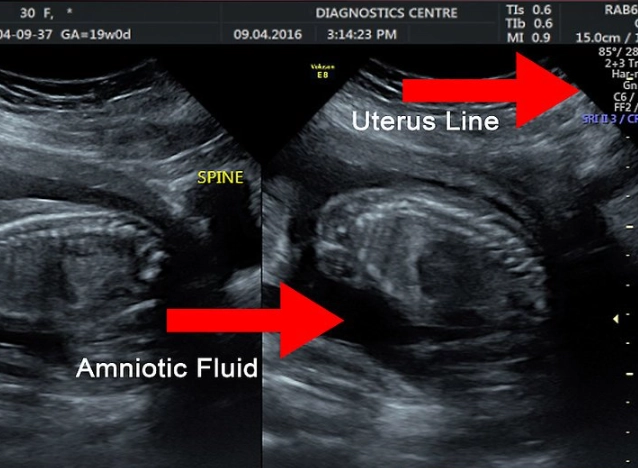
Patient and Exam Information
This is the easy part at the top. It has your name, date of birth, the date of the scan, your hospital ID or medical record number, and sometimes your doctor's name. Double-check this for accuracy—it sounds obvious, but you want to be sure the report in your file is indeed yours.
You'll also see details about the exam itself:
- Type of Ultrasound: Was it a transvaginal (early pregnancy) or transabdominal scan? Sometimes it's both.
- Gestational Age (GA): This is how far along you are, usually calculated from your Last Menstrual Period (LMP) or, more accurately after the first trimester, from the baby's measurements.
- Indication: The medical reason for the scan. Common ones are "routine prenatal screening," "dating scan," "anatomy survey," or "growth scan."
Technical Details and Image Quality
A short note on how the scan went. Phrases like "adequate visualization" or "suboptimal due to maternal body habitus" might appear. The latter isn't a judgment—it just means it was harder to get clear pictures, perhaps due to the baby's position or, quite commonly, because of the mom's build. It doesn't mean something is wrong; it just means some measurements might be estimated.
The Fetal Biometry – The Numbers Section
This is the core of the report and the part most people want to understand. It's a table of key measurements. Here’s a cheat sheet for what they all mean:
| Abbreviation | Stands For | What It Measures | Why It Matters |
|---|---|---|---|
| CRL | Crown-Rump Length | Length from top of head to bottom of torso. | Most accurate for dating pregnancy between 7-13 weeks. |
| BPD | Biparietal Diameter | Width of the baby's head from one parietal bone to the other. | Checks head growth and helps with dating. |
| HC | Head Circumference | Distance around the baby's head. | Assesses brain development and head size. |
| AC | Abdominal Circumference | Distance around the baby's abdomen at the level of the liver and stomach. | A key indicator of fetal weight and nutrition. A small AC can signal growth issues. |
| FL | Femur Length | Length of the thigh bone. | Assesses long bone growth, helps with dating. |
Next to each measurement, you'll see a number (in millimeters or centimeters) and often a percentile. The percentile is the most important part for you to look at. It tells you how your baby's measurement compares to a large population of babies at the exact same gestational age.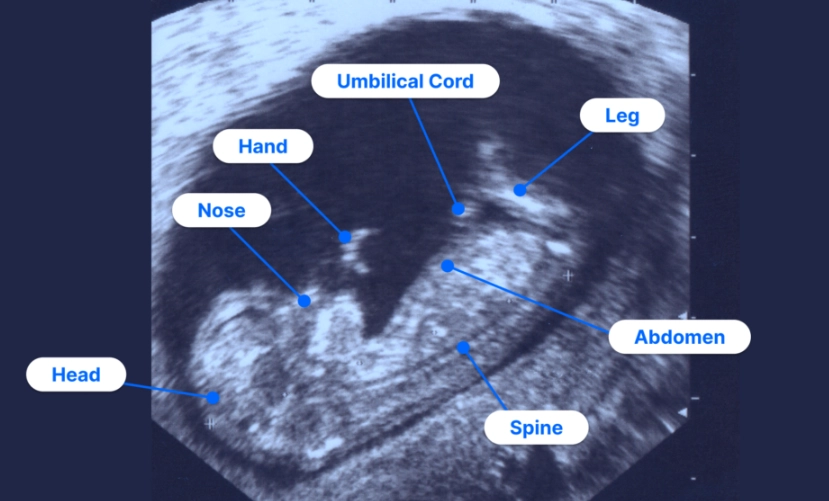
You'll also see an EFW (Estimated Fetal Weight). This is a calculation based on combining the BPD, HC, AC, and FL. It's an estimate, with a typical margin of error of about 10-15%. So, if the EFW is 2000 grams (about 4.4 lbs), your baby's true weight could reasonably be anywhere from 1700 to 2300 grams. This is crucial to remember, especially in the third trimester.
The Anatomy Survey: The "Everything Looks Good" Checklist
This is a narrative section where the sonographer or doctor notes what they visualized. For a standard anatomy scan (around 18-22 weeks), they are checking every major system. The report will often list structures as "visualized," "normal," "unremarkable," or "within normal limits."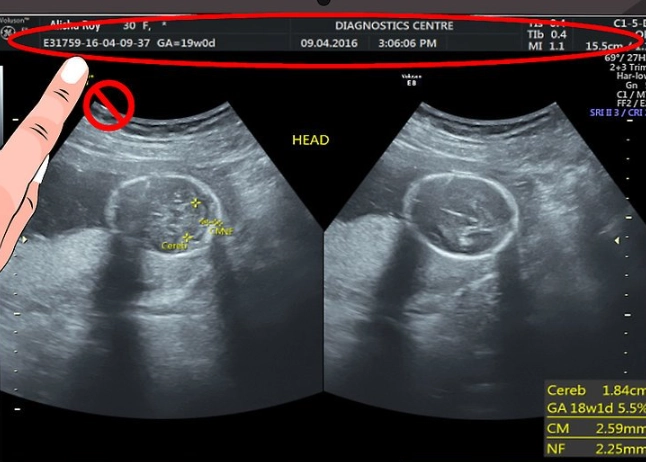
Here’s what they’re looking at:
- Head & Brain: Shape of the head, integrity of the skull, and structures inside the brain like the cerebellum and ventricles.
- Face: Upper lip (to check for cleft lip), profile.
- Spine: Alignment and skin covering along the entire length.
- Heart: This is a big one. They check the four-chamber view, the outflow tracts (the major arteries leaving the heart), and the heart rate/rhythm.
- Abdomen: Stomach (should be visible and filled with fluid), kidneys, bladder, and the abdominal wall.
- Extremities: Arms, legs, hands, and feet. They count fingers and toes if possible.
- Gender: If you chose to find out, it will be noted here.
If something isn't seen clearly, the report might say "not optimally visualized" or "limited view." This usually just means the baby was in a tricky position, and it may need to be checked at the next scan.
Placenta, Amniotic Fluid, and Cervix
This section is about your baby's environment.
- Placenta Location: Where it's attached—like "anterior" (front wall of uterus), "posterior" (back wall), "fundal" (top), or "low-lying." An anterior placenta might mean you feel kicks later or less strongly. A "low-lying" placenta early on often moves up as the uterus grows, but it's monitored.
- Placenta Grade: (0, I, II, III). This describes its maturity/calcification. A Grade III placenta in late third trimester is normal. Seeing it earlier might be noted but isn't always concerning.
- Amniotic Fluid Index (AFI) or Deepest Pocket (DP): Measures the amount of fluid around the baby. Too much (polyhydramnios) or too little (oligohydramnios) can be associated with certain conditions.
- Cervical Length: Sometimes measured, especially if there's a history or concern about preterm labor. A longer, closed cervix is what they want to see.
Impressions, Conclusions, or Recommendations
This is the radiologist's or doctor's summary. It's the "bottom line." It might say:
- "Live, singleton intrauterine pregnancy consistent with [X] weeks gestation." (Great! One baby, right size, growing well).
- "Normal fetal anatomy survey." (The big all-clear from the anatomy scan).
- "Appropriate for gestational age (AGA)." (Growth is on track).
- Recommendations like "Routine follow-up" or "Follow-up growth scan in 4 weeks" if they need to re-check something.

Decoding Common (and Confusing) Medical Terminology
Here’s a quick glossary of terms that often cause a double-take:
- Vertex/Cephalic: Head-down position. Good for delivery!
- Breech/Buttocks: Bottom-down. Very common earlier in pregnancy; many babies turn later.
- Echogenic: Appears bright white on the ultrasound image. Can describe normal structures (bones are echogenic) or sometimes soft markers.
- Soft Marker: A finding that is more common in babies with certain chromosomal conditions but is also frequently seen in perfectly healthy babies. Examples include an EIF (bright spot in the heart) or a CPC (cyst in the brain). They are not abnormalities themselves. Their importance depends on your other screening results (like NIPT or serum screening).
- Ventriculomegaly: Enlargement of the fluid-filled spaces (ventricles) in the brain. Mild cases often resolve on their own; more significant ones need monitoring.
- Pyelectasis / Pelviectasis: Mild dilation of the kidney. Extremely common, usually resolves before or after birth.
- Single Umbilical Artery (SUA): The umbilical cord normally has two arteries and one vein. Having only one artery is a variation. Most babies with SUA are perfectly healthy, but it can be associated with a slightly higher chance of other findings, so it may prompt a closer look at anatomy.
Honestly, some of these terms are unnecessarily scary-sounding. A "choroid plexus cyst" sounds like a brain tumor. In reality, it's a tiny fluid-filled space in a part of the brain that makes spinal fluid, and it almost always goes away by the third trimester with zero impact on the baby.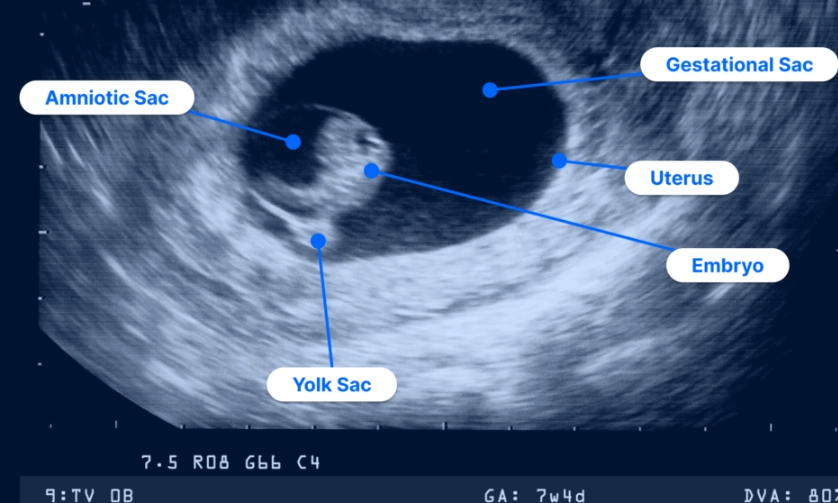
What's Normal? Understanding Ranges and Variations
One of the biggest lessons in learning how to read a pregnancy ultrasound report is embracing the range of normal. Babies, just like people, come in different shapes and sizes from the very beginning.
Let's say all your baby's measurements are between the 30th-60th percentiles. That's beautifully symmetrical growth. But what if the head (HC) is at the 75th percentile and the abdomen (AC) is at the 25th? This is called "asymmetric growth" and might raise a flag. But context is everything. Maybe both parents have large heads. Maybe the baby was curled up, making the AC hard to measure accurately. Your provider will look at the big picture—your health, the placenta, the fluid, and the Doppler blood flow studies (if done).
Doppler studies (not on every report) measure blood flow in the umbilical artery and sometimes other vessels. The key number is the "Resistive Index (RI)" or "Pulsatility Index (PI)." Abnormal flow can indicate the placenta isn't working as efficiently as it could, which might affect the baby's growth. This is advanced info, but if you see it on your report, know it's a tool for monitoring wellbeing.
Questions to Ask Your Doctor After Your Ultrasound
Armed with your new knowledge, you can move from "What does this mean?" to more specific, productive questions. Here are some good ones:
- "Looking at the percentiles, do you see a consistent growth pattern for my baby?"
- "The report mentions [specific term, e.g., pyelectasis]. Can you explain the significance of that in my baby's case, and what is the follow-up plan?"
- "Based on the EFW, how is my baby's size tracking? Does this change my expected delivery plan?"
- "Were all the critical anatomy views obtained, or is there anything we need to try to see better next time?"
- "Do these results align with my NIPT or other screening tests?"
Writing your questions down before the appointment is a game-changer.
Your Ultrasound Report FAQ
When to Seek Clarification (and When to Relax)
It's completely normal to have questions. You should always feel comfortable calling your provider's office to clarify something on your report. That's their job.
However, try to avoid the internet deep dive for every term. I know it's tempting. I've done it. But online forums are full of worst-case scenarios and outdated information. A resource like the American College of Obstetricians and Gynecologists (ACOG) website is a reliable source for general patient information. For more detailed, peer-reviewed explanations of ultrasound findings, professional society sites like the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) have excellent resources. Even the U.S. Food and Drug Administration (FDA) has clear info on the safety and use of ultrasound.
Remember, the vast majority of ultrasound findings are normal or point to minor variations that resolve. The technology is so good now that it picks up on incredibly subtle details, many of which have no clinical impact. Your report is a detailed snapshot, not a final verdict.
Take a deep breath. Look at those little profile pictures. Then, look at your report with this guide by your side. You've got this. Understanding the process is the first step to feeling more confident and less overwhelmed throughout your pregnancy journey.