That question—"How do I know my pregnancy is going well?"—it’s probably on your mind a dozen times a day. You’re Googling every twinge, analyzing every symptom, and just want some reassurance that your baby is doing fine in there. I get it. I spent my first pregnancy in a constant state of low-grade panic, convinced every quiet moment meant something was wrong.
Let’s cut through the noise. A healthy pregnancy isn't about feeling perfect. It's about a series of positive signs, backed by medical checkpoints, that together paint a reassuring picture. This guide won’t just list symptoms; it’ll show you how to read the signals your body and your baby are sending, and, crucially, when to truly relax and when to pick up the phone.
What to Expect in This Guide
- What Are the Early Signs That My Pregnancy Is on Track?
- The Most Reliable Sign: Fetal Movement
- Your Prenatal Checkups: The Gold Standard
- Listening to Your Body: The Good, The Uncomfortable, and The Red Flags
- A Quick-Reference Timeline of Healthy Pregnancy Milestones
- The Bottom Line: When to Stop Guessing and Call Your Provider
What Are the Early Signs That My Pregnancy Is on Track?
The first trimester is a black box. You can't feel kicks, you might not look pregnant, and it’s easy to spiral. The signs here are more subtle and often tied to hormonal shifts.
Breast tenderness that feels more intense than typical PMS is common. Fatigue that knocks you out by 2 PM is your body’s way of saying it’s working hard. And yes, nausea or food aversions, while miserable, are often linked to rising levels of the pregnancy hormone hCG.
But here’s the non-consensus part everyone misses: The absence of these symptoms does NOT mean something is wrong. I’ve had friends with picture-perfect pregnancies who never felt a wave of nausea. Relying solely on feeling sick is a terrible barometer. The real early reassurance comes from your healthcare provider.
A quick note on spotting: Light spotting around the time your period would have been due (implantation bleeding) or after sex or a pelvic exam can be normal. But any bleeding accompanied by cramping, or bleeding that's more than light spotting, warrants a call to your doctor. Don't hesitate.
The Most Reliable Sign: Fetal Movement
Once you start feeling those first flutters (usually between 18-25 weeks for first-time moms), fetal movement becomes your daily check-in. This isn't just a cute bonding experience; it's critical data.
By 28 weeks, you should start paying attention to patterns. Babies have sleep cycles, but they also have active periods. Your job is to learn your baby's routine. Does he bounce after you eat breakfast? Does she have a dance party at 10 PM?
How to Actually Do a "Kick Count" (Without Driving Yourself Crazy)
Forget the rigid "10 kicks in 2 hours" rule if it stresses you out. The American College of Obstetricians and Gynecologists (ACOG) emphasizes noticing your baby's unique pattern and any significant decrease from that norm.
Here’s a simpler method: Pick a time of day when your baby is usually active. Lie on your side, focus, and time how long it takes to feel 10 distinct movements (kicks, rolls, swishes). If it takes longer than usual, or if you feel a dramatic drop in activity, don't wait. Call.
This is non-negotiable: A sudden, significant decrease in fetal movement is the number one reason to contact your provider immediately in the third trimester. Do not drink a sugary drink and wait. Do not tell yourself you're being paranoid. This is the single most important piece of self-monitoring advice I can give you.
Your Prenatal Checkups: The Gold Standard
This is where the rubber meets the road. All the googling in the world can't replace these appointments. They are your objective report card.
First Trimester Confidence Builders
The initial appointments are about confirmation and baseline health. Your provider will likely do a dating ultrasound (confirming a heartbeat and due date) and run blood tests. Seeing that little flicker on the screen is a massive milestone. Blood tests check your hCG and progesterone levels, which should rise predictably in a viable pregnancy.
The Anatomy Scan: Your Mid-Pregnancy Report Card
Around 18-22 weeks, you get the big scan. The sonographer measures everything—the baby's head, abdomen, femur, checks the heart's four chambers, counts fingers and toes, examines the brain, spine, and major organs. They also check the placenta location and amniotic fluid levels.
A normal anatomy scan is a huge sigh of relief. It rules out many major structural issues and confirms baby is growing appropriately.
Third Trimester: Monitoring Growth and Position
Appointments become more frequent. Your provider will measure your fundal height (the distance from pubic bone to top of uterus) to track growth. They'll check the baby's position (head-down is ideal for delivery). They'll monitor your blood pressure for signs of preeclampsia and check your urine for protein.
Steady, appropriate weight gain and a blood pressure reading in the normal range are silent but powerful signs things are going well.
Listening to Your Body: The Good, The Uncomfortable, and The Red Flags
A healthy pregnancy isn't a comfortable one. Distinguishing between normal discomfort and a warning sign is key.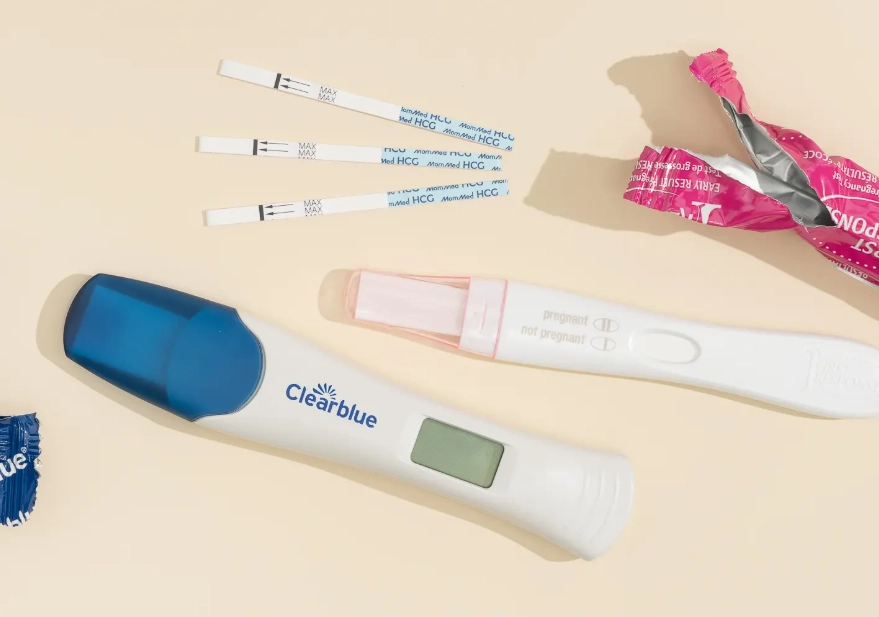
Normal (But Annoying): Round ligament pain (sharp pains in your lower abdomen/groin when you move), mild swelling in feet/ankles later in the day, heartburn, backache, Braxton Hicks contractions (irregular, painless tightening of the uterus).
Red Flags (Call Your Provider):
- Severe abdominal pain that doesn't go away.
- Visual disturbances: Seeing spots, flashes of light, blurry vision.
- Severe headache that won't quit with acetaminophen.
- Sudden, severe swelling in your hands, feet, or face.
- Contractions that are regular and getting closer together before 37 weeks.
- Leaking fluid from your vagina (could be your water breaking).
- No fetal movement or drastically reduced movement.
Your intuition matters. If something feels seriously off, even if it's not on a list, get it checked.
A Quick-Reference Timeline of Healthy Pregnancy Milestones
| Trimester | Key Signs & Milestones | Medical Checkpoints |
|---|---|---|
| First (Weeks 1-12) | Positive pregnancy test, missed period, breast tenderness, fatigue, nausea (or not!). | Confirmatory ultrasound (fetal heartbeat), initial blood work, establishing due date. |
| Second (Weeks 13-27) | Energy returns, "baby bump" appears, first flutters of movement (quickening) begin. | Anatomy scan (18-22 wks), AFP screening, glucose challenge test (for gestational diabetes). |
| Third (Weeks 28-40) | Regular, predictable fetal movement patterns, increasing Braxton Hicks, baby "drops." | Fundal height measurements, fetal position checks, Group B Strep test, more frequent appointments. |
The Bottom Line: When to Stop Guessing and Call Your Provider
After two pregnancies and countless conversations with my OB, the rule is simple: When in doubt, call. Your care team is there for this exact reason. It is never a bother.
They would infinitely prefer you come in for a false alarm than stay home with a real problem. Memorize the red flags, but also give yourself permission to call about anything that's causing you sustained anxiety. Sometimes just describing your symptoms to a nurse can provide instant clarity.
Knowing your pregnancy is going well is a combination of trusting the process (those prenatal appointments), learning your body's and your baby's language (movement patterns), and having a clear line of communication with your healthcare team. Focus on that combination, and you'll spend less time worrying and more time enjoying this unique journey.
Questions You Might Still Have
Is it normal to have no morning sickness in early pregnancy?
Yes, it's completely normal. While often talked about, only about 70-80% of pregnant people experience nausea. The absence of morning sickness does not indicate a problem. A healthy pregnancy is judged by a combination of factors like appropriate hCG hormone rise (seen in blood tests), early ultrasound findings, and the absence of severe pain or bleeding, not by the presence of one specific symptom.
What should I do if I notice a decrease in my baby's movements in the third trimester?
Do not wait. Contact your healthcare provider or go to labor and delivery immediately. A noticeable decrease in fetal movement can be a sign the baby is under stress. Don't talk yourself out of it by thinking the baby is just 'sleepy.' Providers expect these calls and would much rather check on a healthy baby than miss a problem. It's the single most important piece of self-monitoring advice in late pregnancy.
Can a healthy pregnancy have complications later on?
Unfortunately, yes. This is a crucial but tough reality. A pregnancy can be perfectly normal for months and then develop issues like preeclampsia, gestational diabetes, or issues with fetal growth in the third trimester. This is exactly why regular prenatal appointments continue throughout pregnancy. They are designed to screen for these later-developing conditions. A healthy start is a great sign, but it doesn't grant immunity, so maintaining consistent care is vital.